A series of newly installed monitors and instruments silently await
the first round of patients admitted to the EEG Laboratory of the
Epileptology Center video at the Neurological Clinic of the University
of Pécs (PTE). A few years ago, such a high-tech facility would have
been more likely the script of a science-fiction film, as it offers no
less than 24-hour real-time observation of brain activity regarding the
patients admitted here, using EEG (iEEG), an intracranial electrode
placed inside the skull.
The central area of the lab is an ultra-high resolution monitor
covering half of a wall, in which Dr. Márton Tóth observes the
development of epileptic seizures with enormous detail. Special
knowledge is deemed necessary to decipher and find the epileptic foci
which are often concealed from the conventional diagnostic methods.
Following this procedure, those epileptic focis which were pinpointed
are removed by the surgeons aligned to the Neurosurgery Clinic,
resulting in effectively healing a dreaded, stigmatizing disease.
Admittedly, there is a long way to go towards improving patients quality
of life and comprehensively training medical staff seeking to heal
them.
"Morbus Sacer": The Sacred Disease, or the Curse of the Gods
It is worth starting with the basics. Epilepsy is caused by a
defective area of the brain, the commonly referred to epileptic foci.
This area triggers attacks by an increased discharge of nerve cells,
causing a "system shock". Repetition is an important condition of the
disease, as there may be other kinds of epileptic seizures which are
caused by an external effect (such as a stroboscope) or a serious
illness, and fortunately, are not permanent. The epilepsy-causing foci
occur for a variety of reasons, some of them are genetically inherited
or caused by developmental disorder. Additionally, epilepsy can develop
any time leading to permanent lesions due to major accidents and
illnesses.
Approximately one percent of the world's population, nearly 100,000
individuals throughout Hungary, are currently suffering from the
disease, which can cause enormous damage with immediate consequences,
often resulting in serious injuries and in extreme cases, cardiac
arrest. "It is difficult to say the exact number of patients since
epilepsy is a daily stigma, which is often concealed by sufferers and
their families, because patients are often stigmatized by society," says
Dr. Tóth, who specializes in the treatment of illness. He also informed
us, in which those afflicted with epilepsy, the rate of depression and
suicide is 25 times more frequent.
The good news is in consideration of today's traditional methods,
60-70 percent of patients treated result in symptom-free by medication,
and a good portion of the remaining patients, nearly 3,000 to 6,000 in
Hungary, undergo treatment in which the foci are surgically removed. The
sad news is the number of epileptic patients remains largely unchanged.
For some yet unknown reason, the epileptic foci in an increase among
patients undergoing conventional diagnostic methods, primarily skull MRI
and PET, including an EEG on the skull, are unable to identify.
However, the new intracranial EEG offers help in these situations.
Detecting the Hidden Foci
There are many types of epilepsy, generally dependent upon the
location of the foci within the brain and corresponds to the various
causes of seizure. One type is the commonly known drug-resistant
variety, which develops as a result of fever spasms during childhood, in
which the focal point of the disease is relatively easy to find and
remove. Over the past decade, however, epileptologists around the world
have found increasing numbers of cases in which the developmental
disorders leading to epilepsy are non-detectable using the conventional
MRI.
The evolution of medical technology and the ever-increasing demand
has led to the development of the iEEG, which monitors brain function
and the course of seizures through real-time, offering enormous detail
through the electrodes placed inside the skull. The trained physician is
able to locate the focis, which are normally hidden in the conventional
MRI and PET examinations, and then can be surgically removed. At
present, there are at least a thousand patients throughout Hungary who
cannot be reliably diagnosed using conventional methods, however, in
consideration of the iEEG, there is a relatively good chance (70-75%) of
detection, surgical extraction and recovery.
Admittedly, the method appears simple and as of yet, requires a
significant amount of professional knowledge and extremely sophisticated
instrumentation, since apart from placing electrodes within the
patient's skull, the entire procedure requires several days, even up to
weeks, to effectively study the nature of seizures. Paradoxically, the
greater the seizure frequency represents an advantage regarding the
patient.
Distinctly, intervention can only be implemented within specialized
epilepsy treatment centers, of which, there are only two currently
operational in Hungary, one in Budapest and one in Pécs. One of the
former often-referred to subdural forms of the procedure was first
performed at the National Institute of Clinical Neuroscience (OKITI). In
the case of subdural iEEG, a portion of the skull is first removed, and
electrodes are placed directly upon the surface of the brain.
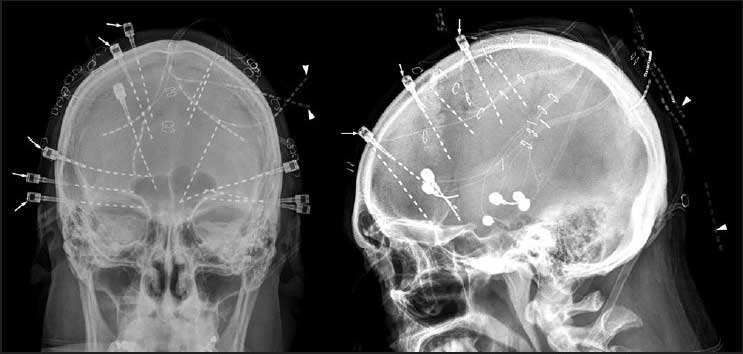
Dr. Márton Tóth, brought home the commonly-known stereotaxic EEG
(SEEG) from Lyon, France, one of Europe's leading epileptic centers,
following an intensive half-year study mission. This method first begins
with miniscule holes (less than one millimeter in diameter) drilled on
one or two sides of the skull, in which electrodes are inserted deep
into the brain.
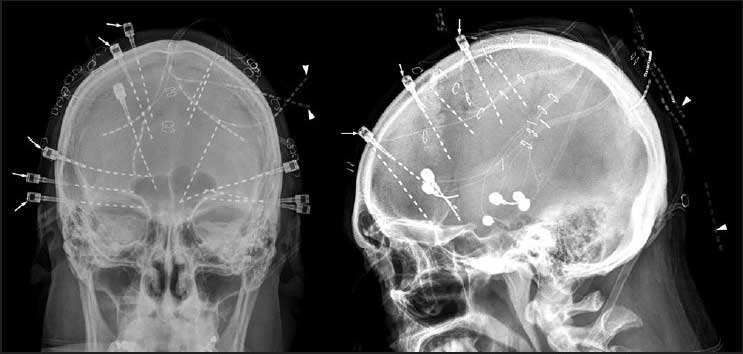
SEEG has far fewer complications, it is less painful and heals much
faster, yet requires tremendous expertise and precision, in reference to
the user. The skilled neurologist strategizes the intended position of
the electrodes after lengthy consideration, which is then followed by
several hours of intense surgical procedures, during which the prepared
neurosurgeon positions the electrodes. A deep trust among the
neurosurgeon and the neurologist is essential towards assuring success.
Dr. Márton Tóth remarks, “In addition to a good working relationship,
you also need to have a friendly relationship in which the complex and
very sensitive interventions can smoothly proceed. The basis of the
surgical procedure is not complicated, it can be compared to a biopsy
(taking a tissue sample from the brain using a needle). The challenge is
primarily to get in touch with the brain at various points and to
ensure we do not unintendedly inflict damage in critical areas such as
brain vessels. All this requires intensive and long-term concentration,
since such an operation requires up to six to seven hours,” says Dr.
Zsolt Horváth, who made the first SEEG surgery in Pécs.
Journey into the Brain
In addition to the human factor, technology is also very important.
For information regarding the brain and nervous system, neurosurgeons
use often-referred to neuron navigational systems, which, as Dr. András
Büki, Director of the Neurosurgery Clinic of PTE, function very much
like the navigation system of a new car, ‘only’ the road network is the
human brain.”
The "map" of the brain is made by high-resolution MR images. During
intervention, the medical team knows on this basis of which area they
are in pursuit of and thus they can avoid damaging critical brain
tissues. There are, of course, difficulties encountered. In contrast to
the largely static road network, the brain recalculates itself during
the intervention, such as the removal of a tumor, and the map falls
apart. All this should be corrected during surgery.
The insertion of deep electrodes requires tremendous precision,
literally tenths of a millimeter, yet, as Dr. András Büki emphasizes,
“It is inherent and synonomous to the task at hand.” The neuronal
navigation system used in SEEG procedures was procured and is valued at
or nearly 300 million HUF, and was financed by a GINOP application.
Reportedly, it is one of the most advanced systems throughout the entire
Central and Eastern European region.
The first successful surgery was carried out on a young patient
culminating in various results from different imaging studies regarding
the precise location of the foci. Dr. Márton Tóth emphasizes, “In this
case, it was not an exaggeration to use the term "fate", since a female
patient, in her twenties, was suffering from continuous night seizures.
The possibility of the patient ever becoming pregnant was contingent on
the success of the procedure.”
Since the traditional EEG, MRI and PET examinations in reference to
the skull had varied results, only the deep electrode examination was
able to answer the exact question of where the foci responsible for the
seizures was located. The intervention was carried out with the help of
French doctors and revealed new dimensions regarding the human brain.
“We could see exactly how the seizure starts and then spreads from
brain to brain area. By doing so, we have been able to determine exactly
where and how much area should be removed.” Today, the patient is
remarkably free from seizures.
A Real Innovation
The goal now is to ensure SEEG operations and tests are sustainable
and to introduce them throughout Hungary. The cost of the first
intervention was nearly eight million forints and financed by the PTE
Chancellery. Preparations for further surgeries are already underway,
yet adequate funding is essential in support of those patients waiting,
and a detailed cost-effectiveness analysis has been carried out by the
PTE's Health Technology Assessment Center.
“When applying for a new type of intervention, it must be
substantiated in which the cost, or financial burden is not unbearably
high, and in going forth with the procedure, patients within reason, can
expect some increase in the quality of life and their life expectancy.
The analysis of the existing data revealed the life expectancy of
epileptic patients will be significantly longer with the SEEG (6-7 years
more) and their quality of life will undergo significant improvement,
at relatively low costs. In quantification, this means we can provide
the patient with a full-quality life span at the expense of nearly one
and a half million forints, which is far below the 9 million cost limit
prescribed by law,” states Dr. Antal Zemplényi, Head of the Health
Technology Assessment Center.
The calculation was also confirmed by the national professional
organizations, and the application for funding is awaiting ministerial
judgement. In the event of a favorable evaluation, a total of 48
interventions will be carried out annually, and performed in the two
Hungarian centers. "A genuine innovation is a social benefit, and the
introduction of SEEG throughout Hungary can be a model in this respect,"
offers Dr. Tamás Dóczi, Academician, Head of the Clinical Research
Pillar of the National Brain Research Program. "Of course, there will be
no Nobel Prize, yet we can help thousands of untreatable patients thus
far, and this is real medical innovation."